Popust Jednobojnu ženska Torba Na Rame Male Torbe Preko Ramena Torbe Moda Umjetna Koža 2021 Modni Trend ženska Torba Na Rame > Ženske torbe ~ Dom-blato.com.hr

Umjetna Koža Torbe, ženske Berba Velike Torbe, ženske Torbe Preko Ramena Smeđe ženske Kožne Torbe Svakodnevni Torba ženski Ručni Velike Torbe kupiti | Ženske Torbe - Sultan-drinks.com.hr

2021 nova modna ženska torba-instant messenger mali trg torbe, ženske crnci smeđe torbe na rame jednog veličine ženske torbe velikog kapaciteta | Popust > www.plavatavavarazdin.com.hr

Popust Smeđe ženske Torbe Za Skitnice 2021 Zima Novi Trend Kvaliteta Umjetna Koža Torba Preko Ramena ženska Svakodnevni Torba-instant Messenger ženska Torba Na Rame ~ Ženske Torbe < www.ekstenzije-trepavica.com.hr

Nove ženske torbe na ramena, od prirodne kože Luksuzni Dizajn Klasične ženske torbe sa širokim remenom od bičevati Torba-instant messenger Torbice smeđe boje kupi online | Ženske torbe - www.metalstil.com.hr

Kupiti Prirodna Koža žene Lanca Torbe Na Rame Kvalitetan ženski Veliki Retro Torbe Dame Kravlja Koža Smeđe Torbe Bolsa Mujer ~ Ženske Torbe - Bajka.com.hr

Starinski dizajn, ženska mala torba na rame, smeđi leptir s vezom, ženske torbe ispod pazuha, trendy cool torbe-skitnice za djevojčice, torbice, torbe poredak / Ženske torbe < Bioptron.com.hr

Kupiti Svakodnevne Smeđe Torbe-Тоут, Kvalitetne Ženske Torbe Na Ramenu Od Umjetne Kože, Skup Velikih Вместительных Putne Torbe, Ženske Monotono Torba Za Kupovinu - Ženske Torbe > www.autoplinbubic.com.hr

Smeđa vintage funky svakodnevni torba-тоут бостонские ženske torbe poznatih brandova luksuzna ženska torba od umjetne kože ženska torba na rame yz-23 kupi online | Ženske Torbe < www.cateringkodane.com.hr

2020 stare smeđe ženske kožne torbe luksuzne dizajnerske torbe na pojas visokog kvaliteta marke crossbody torbe za žene bolso mujer kupi online - Ženske torbe > Jeftinaputovanja.com.hr

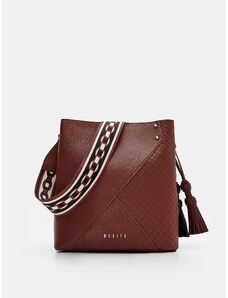
2022 Marke Design ženska torba-kantu od prave kože Ženske torbe Visoke kvalitete Ženske Torbe na rame Novi Luksuzni torbu smeđe boje kupi online / Ženske torbe \ Some.com.hr

Cnoles ženske Torbe Na Rame Dizajnerske Torbe Od Prave Kože Torba Preko Ramena Male ženske Torbice ženski клатч poredak | Ženske Torbe - Kjtranslations.com.hr

2023 Berba ženske Torbe Na Rame, Svakodnevne Dizajnerske Smeđe Torbe Preko Ramena Od Umjetne Kože, ženske Luksuzne Marke Jednostavne Torbe I Torbice kupiti | Ženske Torbe \ www.strojevi.com.hr

Modni Dizajner Smeđa ženska Torba Velike Torbice, Torbe Europske Torbe Na Rame Klasicni Ulje Vosak, Koža Je Velika Torba > Ženske Torbe < Mreznicarun.com.hr